Jessica Yaniv, a trans woman from Canada, has reignited debate over transgender healthcare access after claiming she was refused treatment by a gynecologist simply because of her gender identity. Her public complaint, which follows previous controversies, once again places her at the center of a broader conversation: What happens when trans patients seek care doctors may feel unqualified—or unwilling—to provide?
According to Yaniv, the rejection came with few words: “We don’t serve transgender patients.” She shared her experience on social media, saying she felt “shocked, confused, and hurt.” Tagging the College of Physicians and Surgeons of British Columbia, she questioned the legality of the refusal. While she initially claimed the College confirmed it was discriminatory, the regulatory body later clarified it does not offer opinions on individual cases over the phone, instead directing patients to existing practice standards.
Yaniv didn’t reveal the exact care she was seeking, but the case is already drawing comparisons to similar incidents globally. From France to the U.S., medical providers have echoed a recurring sentiment: “I don’t feel qualified.” In one French case, a doctor turned away a trans woman but offered to refer her elsewhere—until his comment about treating “real women” stirred backlash and led to a public apology.
This isn’t the first time Yaniv has taken legal action over alleged discrimination. In 2019, she made headlines after filing complaints against Vancouver-area beauty salons that refused to perform Brazilian waxes on her male genitalia. Those cases were ultimately dismissed, with a human rights tribunal ruling her motives appeared more aligned with personal financial gain than the fight for equality.
Still, Yaniv’s newest complaint reopens critical questions: What rights do trans patients have? And what obligations do doctors hold when facing care requests they’re not trained to handle?
Medical experts highlight that while trans women may seek gynecological care post-surgery, routine exams—like Pap smears—are generally unnecessary unless complications arise. Neo-vaginas created through gender-affirming surgery differ significantly from natal female anatomy, often requiring specific post-operative knowledge many gynecologists don’t receive in standard medical school training. “You can’t treat what you don’t understand,” one doctor noted, emphasizing that discomfort or lack of training should lead to referral—not rejection.
Yaniv’s case spotlights a gray area between discrimination and clinical limitation. Canadian laws vary by province, but in general, refusing care based solely on identity is illegal. Declining a procedure due to lack of training, however, can be considered appropriate—so long as a patient is offered a timely referral.
But in reality, transgender patients often fall through the cracks.
Research shows nearly one in four transgender people delay or avoid medical visits out of fear of mistreatment. In one tragic case, a transgender man faced multiple rejections from gynecologists before finally securing care—by then, it was too late. He was diagnosed with ovarian cancer after a year-long delay.
Medical educators argue the solution isn’t simply expecting all doctors to be experts in transgender health, but creating systems where providers know when and how to refer—without bias. “It’s not enough to say ‘I don’t know,’” a healthcare director explained. “But it’s also okay to say, ‘This needs a specialist, and here’s who can help you.’”
The conversation around transgender healthcare is growing as more people seek medical transition support. In Europe, reported cases of gender dysphoria increased tenfold between 2013 and 2020. With demand rising, the pressure is on medical institutions to balance respect for patient identity with the reality of specialized care.
As Yaniv’s complaint remains under review, it underscores the urgent need for clear policies and compassionate practice. For many trans patients, the question isn’t just whether care is available—but whether it’s truly accessible.
And for healthcare systems around the world, this isn’t just a matter of procedure—it’s a test of principle.
News
DOLLY PARTON’S $20 MILLION PROMISE: THE COUNTRY LEGEND WHO TURNED GRIEF INTO GRACE — AND REKINDLED AMERICA’S FAITH IN LEGACY
THE CALL THAT CHANGED EVERYTHING The morning it broke, America didn’t quite know what to do with itself.No scandal. No…
THE FOOTAGE THEY TRIED TO ERASE: THE FINAL MINUTES OF CHARLIE KIRK — AND THE DOCTOR WHO BROKE HIS SILENCE
THE VIDEO THAT SHOULDN’T EXIST It began at 3:14 a.m. — with an upload to a private Telegram channel called…
The Betrayal of a Patriot: A Cinematic Conspiracy Unraveled
The stage was set in the heart of Phoenix, Arizona, under a blazing desert sun. The air crackled with anticipation…
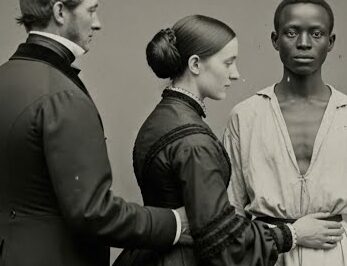
The 𝐇𝐞𝐫𝐦𝐚𝐩𝐡𝐫𝐨𝐝𝐢 Slave Who Was Shared Between Master and His Wife… Both Became Obsessed (1851)
In the sweltering August of 1851, the tobacco fields of Southside Virginia held secrets far darker than the thick red…
Rich Young Master Spends Money To Force Black Maid To Crawl Like A Dog Just For Fun – Her Reaction Shocks Everyone…
Morning in Bell Ridge always arrived polished—dew on clipped lawns, a flag snapping above City Hall, white magnolias leaning over…
She Was Fired for Helping a Veteran’s Dog! Minutes Later, Marines Stormed the Café
The morning light over Mason, Georgia, looked cooler than it felt—silver on storefront glass, a flag lifting over the courthouse,…
End of content
No more pages to load